Contusion or bruises happen when small blood vessels under the skin are damaged, causing blood to leak into surrounding tissues and resulting in discoloration and tenderness. Commonly arising from minor falls or sports injuries, most bruises heal on their own. However, large or deep bruises can indicate more serious issues like internal bleeding disorders or hematomas, which may require medical attention. Recognizing the severity of bruises is crucial; while small bruises are often harmless, those that grow in size, appear without trauma or cause severe pain should be monitored closely and may need urgent evaluation. Understanding when to seek care ensures proper attention to potential injuries.
In this blog, you’ll learn about bruises and different colors, stages, and when to see a doctor.
The Biology of Bruising
When an impact occurs, such as a fall or a bump, it causes immediate damage to the skin and underlying tissues. Bruises form results in the rupture of capillaries—tiny blood vessels that supply oxygen and nutrients to tissues. The rupture causes body breaks that lead to blood leakage into the surrounding tissue, forming a bruise, also known as a contusion. According to the American Academy of Family Physicians, around 75% of people experience bruising at some point in their lives, often due to minor trauma. As the capillaries break, blood escapes into the interstitial space (the area between cells), leading to the characteristic discoloration and swelling associated with bruises. The initial response to injury involves vasoconstriction, where blood vessels constrict to minimize blood loss. However, as damage persists, coagulation begins, wherein the body forms a clot to stop further bleeding.
The Stages of Bruises Healing
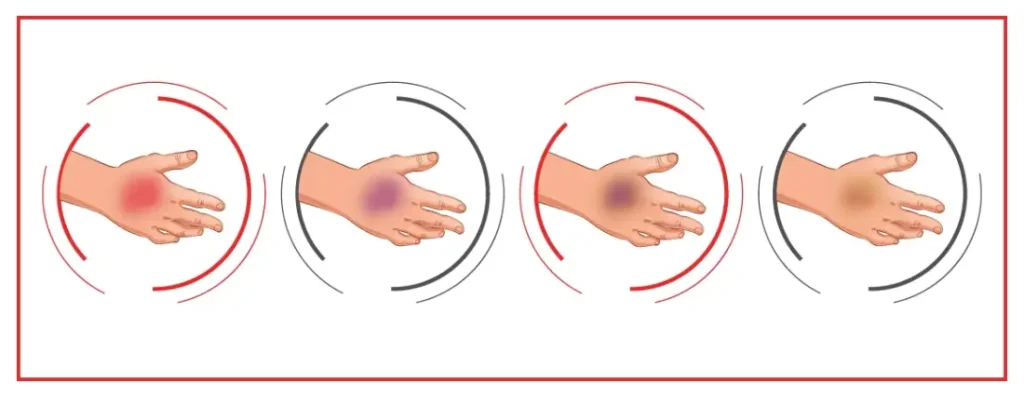
Bruise healing occurs in several stages:
- Initial Stage (Red/Purple): Immediately after injury, the bruise appears red due to fresh blood pooling beneath the skin. This can quickly turn purple as hemoglobin (the oxygen-carrying component of red blood cells) degrades.
- Blue Stage: Within 1-2 days, the bruise may turn a deep blue or purple color as the blood continues to leak into tissues. This stage is indicative of ongoing tissue damage.
- Green Stage: As the body starts to break down the hemoglobin, the bruise may shift to a greenish hue due to the presence of biliverdin, a pigment formed from hemoglobin breakdown.
- Yellow Stage: Finally, the bruise may appear yellow as the body continues to metabolize the pigments. This occurs when the bruise is healing and the blood is being reabsorbed by the body.
Throughout these stages, the body produces collagen and other substances to repair the damaged tissue, signaling the completion of the healing process.
Different Types of Bruises
Bruises can vary by depth and severity:
Minor Bruises: Common, surface-level, caused by minor bumps. Appear red, purple, black, and blue marks, healing in 1-2 weeks without treatment.
Hematomas: Blood pools outside vessels, causing raised, swollen bruises. Can result from deep trauma, sometimes needing medical attention.
Subcutaneous Bruises: Occur in the fat layer beneath the skin. Larger and often swollen, they take longer to heal.
Deep Tissue Bruises: Affect muscles, may not be visible, but cause pain and limited movement. May require medical care if severe.
Dangerous Bruises Based on Color
Bruise color changes indicate healing stages and potential severity:
Color Progression:
- Red: Fresh injury, blood pools.
- Purple/Blue: Deoxygenated blood, normal for several days.
- Green: Healing stage, breakdown of hemoglobin.
- Yellow/ light Brown: Final stage, after 1-2 weeks, the bruises most likely be a light brown.
Warning Signs:
- Black and Blue Marks: Possible severe trauma or hematoma, needs attention if painful or swollen.
- Deep Purple: This could suggest internal bleeding.
- Unexpected Green: May indicate complications.
Monitor bruise colors to assess healing and decide if medical care is needed.
Large or Spreading Bruises
Large or expanding bruises can signal serious underlying conditions. Larger bruises often indicate significant trauma, internal bleeding, or damage to muscles and organs, and can lead to complications like hematomas, which may require surgery. According to the National Health Service (NHS), up to 50% of serious injuries result in significant bruising.
Signs of a dangerous hematoma include:
- Increasing size – continuous bruise expansion suggests ongoing bleeding.
- Severe pain – intense pain may indicate deeper injury.
- Swelling and darkening – rapid changes in size or color need urgent attention.
Spontaneous bruising without trauma can signal clotting disorders or conditions like liver disease, warranting immediate medical evaluation.
Bruises That Indicate Internal Bleeding
Bruises can sometimes indicate internal bleeding, especially if they occur in unusual areas like the abdomen or back. Deep bruising or abnormal color changes may suggest more severe underlying issues.
Signs of internal bleeding include bruises that don’t follow typical color progression, accompanying symptoms like pain, swelling, dizziness, or weakness, and may require immediate medical attention.
Diagnosis involves a medical evaluation, imaging tests (ultrasound, CT scans), and blood tests to assess internal damage and blood clotting.
Bruises and Blood Disorders
Spontaneous bruising can signal underlying blood disorders. Key conditions include hemophilia, where clotting is impaired, and leukemia, which leads to low platelet counts, causing frequent bruising. Other disorders like von Willebrand disease also disrupt clotting, making bruising more common.
Warning signs include unexplained or frequent bruising, large or unusually colored bruises, and accompanying symptoms like prolonged bleeding or nosebleeds. Diagnosis involves blood tests (CBC, clotting factor assays), bone marrow exams for suspected leukemia, and coagulation studies (PT, aPTT) to assess clotting efficiency.
Medications and Bruising
Certain medications can cause bruising, especially those affecting blood clotting and tissue strength. Blood thinners like warfarin and aspirin increase the risk of bruising by reducing clotting ability. Combining blood thinners with other drugs like NSAIDs can heighten this risk. Corticosteroids, such as prednisone, also weaken skin and blood vessels, leading to easier bruising. Some antibiotics and cancer treatments may have similar effects.
It’s important to discuss all medications with your doctor, especially if you notice frequent bruising. Regular monitoring and possible dosage adjustments can help manage these side effects safely.
Bruises and Aging
Aging skin thins and blood vessels become more fragile, increasing the likelihood of bruising. The loss of collagen and subcutaneous tissue makes the skin weaker and less cushioned, leading to easier bruising from minor impacts. A common condition in older adults, senile purpura, causes large purple bruises without significant trauma due to capillary fragility.
Certain medications, such as anticoagulants and corticosteroids, can worsen bruising. Seek medical attention for large, unexplained bruises form, especially in sensitive areas, or if accompanied by symptoms like dizziness or fatigue, to rule out serious issues.
Bruises from Physical Abuse
Recognizing bruises that may indicate physical abuse is essential for ensuring safety and supporting victims. Understanding the patterns and locations of such bruises can help identify non-accidental trauma and facilitate intervention.
Bruises from Non-Accidental or Physical Trauma
Non-accidental trauma refers to injuries from intentional harm, commonly seen in domestic or child abuse. These bruises differ from typical accidental ones and often display distinct characteristics. According to the CDC, around 41% women and 26% men experience severe intimate partner physical violence, highlighting the importance of awareness.
Abuse-related bruises may be more extensive, clustered, or found in unusual locations. They can exhibit patterns indicative of objects or hands, known as “patterned bruising.”
Common Locations of Abuse-Related Bruising
- Arms and Forearms: Bruises in these areas may indicate defensive wounds from attempts to protect oneself, suggesting repeated abuse.
- Back and Spine: Bruises in less accident-prone areas may indicate forceful strikes or restraints.
- Neck and Face: Bruising around the neck may signal strangulation attempts, while facial bruises often indicate severe physical abuse.
- Other Areas: Bruises on the thighs, abdomen, and buttocks may be concealed by clothing.
How to Seek Help and Report Abuse-Related Bruising
- Recognizing Signs: Unexplained bruises, especially in patterns or unusual locations, can indicate abuse or broken bone. Other warning signs include behavioral changes and frequent medical visits for injuries.
- Documenting Evidence: Keeping records of bruises, including photographs and descriptions, can help when reporting abuse.
- Finding Support: Reach out to trusted individuals or professionals for support. Hotlines and local shelters can provide immediate assistance.
- Reporting Abuse: Contact local law enforcement if in immediate danger. For children, report to child protective services to ensure safety.
- Professional Help: Healthcare professionals can evaluate injuries, provide care, and guide individuals through reporting and support processes.
Bruises and Nutritional Deficiencies
Diet significantly impacts overall health and the body’s ability to heal, including its susceptibility to bruising. Certain nutritional deficiencies can lead to easy or unexplained bruising, highlighting the importance of a well-balanced diet.
Vitamin Deficiencies Leading to Easy Bruising:
- Vitamin C Deficiency: Essential for collagen synthesis, a lack of Vitamin C weakens capillaries, making them prone to damage and bruising. Severe deficiency can result in scurvy, with symptoms like bleeding gums and fatigue. According to the National Institutes of Health (NIH), 10% of the U.S. population has inadequate Vitamin C intake.
- Vitamin K Deficiency: Important for blood clotting, Vitamin K deficiency impairs coagulation, increasing bruising risk. This may result from malabsorption or a diet low in green leafy vegetables. According to the NIH, up to 40% of older adults may be Vitamin K deficient.
- Other Nutritional Factors: Deficiencies in B vitamins and zinc can also contribute to easy bruising, affecting skin health and healing.
Nutritional Solutions:
- Incorporate Vitamin-Rich Foods: Consume foods high in Vitamin C (e.g., citrus fruits, berries) and Vitamin K (e.g., spinach, kale).
- Balanced Diet: Focus on a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats to ensure adequate nutrient intake.
- Nutritional Supplements: Consider supplements for those with absorption issues, after consulting a healthcare provider.
When to Consult a Doctor:
- Frequent or Unexplained Bruising: If bruising persists despite dietary changes, consult a healthcare professional to rule out underlying health issues.
- Symptoms of Nutritional Deficiency: Seek medical advice for additional symptoms like fatigue or skin changes. Blood tests may be necessary to identify deficiencies.
- Potential Underlying Health Issues: Easy bruising could indicate conditions like clotting disorders or liver disease, requiring evaluation and guidance from a healthcare provider.
When to Seek Medical Attention for Bruises
While bruises are typically harmless, certain signs indicate when medical attention is necessary. Seek care if a bruise doesn’t heal within a few weeks, is unusually painful, appears without cause, or if multiple bruises in different stages of healing occur. Accompanying symptoms like fatigue, weight loss, or fever also warrant evaluation.
Individuals with conditions like hemophilia or liver disease, older adults, and those on blood thinners should monitor changes in bruising. Medical evaluations may include blood tests and imaging to assess for underlying issues, with specialist referrals as needed.
Frequently Asked Questions
How to heal a bruise?
Apply a cold compress for 15-20 minutes to the bruised area several times a day, keep the area elevated, and use over-the-counter pain relief to help heal a bruise faster.
How long does it take for a bruise to go away?
Bruises typically take 1-2 weeks to heal, depending on their severity, location, and overall health.
Does ice help bruising after 3 days?
A cold compress can help reduce swelling within the first 48 hours, but after three days, it's better to use a warm compress to improve circulation and healing.
What deficiency causes easy bruising?
Easy bruising can result from deficiencies in vitamins C, K, and B12, as well as certain conditions like platelet disorders or liver disease.
When should you worry about a bruise?
Consult a doctor if bruises appear without injury, are very painful, or if you experience frequent bruising alongside other unusual symptoms.
What causes small blood vessels to bleed?
Small blood vessels can bleed due to trauma, such as bumps or falls, or conditions like vascular diseases that weaken vessel walls, leading to leakage.
What blood cells cause bruising?
Bruising is primarily caused by red blood cells leaking into tissues after blood vessels are damaged, which creates the characteristic discoloration.
Does blood flow help bruises?
Blood flow helps in healing bruises by delivering nutrients and oxygen to damaged tissues, promoting recovery and reducing inflammation.
What are other similar types of bleeding?
Several types of bleeding disorder cause skin discoloration, including:
Hemorrhage: Excessive blood loss from damaged blood vessels.
Petechiae: Tiny red or purple spots caused by bleeding under the skin.
Ecchymosis: Larger areas of discoloration similar to bruises.
Hematoma: A localized collection of blood outside blood vessels, often raised and swollen.
– Disclaimer –
This blog is for informational & educational purposes only, and does not intend to substitute any professional medical advice or consultation. For any health related concerns, please consult with your physician, or call 911.
-
About The Author
Dr. Syra Hanif M.D.Board Certified Primary Care Physician
Dr. Syra Hanif is a board-certified Primary Care Physician (PCP) dedicated to providing compassionate, patient-centered healthcare.
Read More